EDITORIAL
Osteoarthritis from different points of view
In 20 years, advances in modern medicine have wiped out many diseases and increased lifespan.
Modern therapeutic possibilities by synthetic drugs with an infinity of substances, seem to face the disease like an army of warriors, ready for the supreme battle where there is only one winner. But besides that, there is a less aggressive and more merciful medicine which will consider man and his disease as an entity, the disease no longer resulting from a break-in or intromission, but from a decrease in strength. and weakening. It is therefore no longer necessary to attack the evil, which, by ricochet, defeats the patient but it is more appropriate to raise the patient, to restore his balance and his lost harmony.
Nature, this inexhaustible reservoir of strength, has always offered us all the beneficial substances on condition that they are chosen wisely.
More than one in two people in France, after 60 years, consult for joint pain, which is the leading cause of consultations in general practice. For all those who suffer from osteoarthritis, we have made the judicious choice of this other way of taking charge of the disease and its disorders, to raise, restore and harmonize such or such joint while remaining attentive to the entity of the to be, keeping for objective the well-being of the individual which could not be global.
For osteoarthritis, this joint disorder qualified as a disease but which is not one – no microbe or bacteria against which to fight – the association of a recognized chondroprotector and powerful anti-oxidants open a new path of restoration joint function lacking side effects. A modern era is dawning when the increase in the life expectancy of the population will confront us with an increasing number of patients asking us to help them in the management of their functional deficits.
We took the gamble of responding present and always offering a coherent, non-aggressive, natural and comprehensive solution to this major public health problem.
This is a priority for us, as have national and international bodies which have classified the coming decade as that of bones and joints.
Doctor Roger LECURIEUX-CLERVILLE
ARTHROSIS
Mechanical etiology by Doctor René HERNANDEZ
Rheumatic pains are one of the main causes of consultation in general medicine.
Degenerative rheumatism such as osteoarthritis is constantly increasing, it is the most common joint disease, it affects about 9 million French people, or 70% of the population aged over 65 and the increase in Unfortunately, life expectancy is not accompanied by an improvement in living comfort.
Osteoarthritis is a chronic degenerative condition of the joints that undergo progressive wear and tear which is complicated by pain accompanied by disabling functional impotence. Against this background of pain and stiffness, bone deformities appear and the disease progresses sometimes through inflammatory flares.
Joint is movement, that is, the mobility and mobilization of bones.
The mechanical stresses of movement are supported by the joint and more particularly by one of the structures of the joint, the articular cartilage that covers the bone ends. In osteoarthritis this is the element that is affected first, this crusty cartilage that cracks, becomes rough and wears down.
As a result, the joint seizes up. Then the surrounding bone lesions present either as hardening of the bone (condensation), or with cavities (geodes) or both.
Around the edges appear osteophytic “parrot beak” spikes, self-defense phenomena. Finally, there may be a hardening of the synovium.
Normal articular cartilage is a very differentiated connective tissue, devoid of vessels and nerve, it makes movement easy and imperceptible because it does not contain a nerve, so it cannot transmit any information to the brain (this function is devolved to the periarticular structures, ligaments and tendons).
Its function is twofold:
• Allow the transmission and absorption of loads on bones throughout life.
• Reduce the friction generated by the friction of the two bones by ensuring the sliding of the bone ends with a very low coefficient of friction.
Imagine two perfectly smooth, flat, slightly damp ice cubes sliding against each other, smoothly without ever getting stuck. Now consider a surface 8 to 10 times more slippery than ice, this is our cartilage. The articulated bony ends are united in a joint called a diarthrose whose structures are held together by strong ties:
- The capsule (connecting the two bones)
- The synovial membrane (fibrocellular membrane which lubricates and nourishes the cartilage) It develops and secretes hyaluronic acid (and lubricating glycoproteins)
- Ligaments (attach and stabilize)
- Tendons and muscles (secondarily attach and stabilize)
- Serous bursae (protect tendons and ligaments)
- Blood supply (veins-arteries-lympahatics)
- Innervation (proprioceptive sensors)
- In some diarthroses (knee for example) there are other important structures such as menisci and intra-articular ligaments.
All the movements we make are a succession of incomplete gestures that the body must constantly compensate for. It changes the spinal curvature, contracts different muscle chains, relaxes other planes, corrects the direction of body lines.
This cascade of “accidents” affects the mobility of structures.
During certain prolonged postures or joint forced actions, it appears in the tissues, pain which considerably interferes with the proper functioning of joint dynamics. These pains are localized at the level of muscle insertions, that is to say at the level of the tendons; these zones are subjected to a maximum of tension; thus joint function is disturbed:
• It ensures the maintenance of a balanced attitude of the joint in a determined position.
• It poorly ensures the harmonious mobilization of the skeletal parts present within the limits imposed by the anatomical and physiological characteristics of the joint considered.
The control of joint mobility is carried out from sensory receptors, manifests itself at the level of receptors and is organized in tiered nerve centers:
Sensitive receptors:
- Rufini receptors in joint ligaments are receptors for information about the speed and direction of movement.
- The GOLGI articular corpuscles, at the level of the ligaments, are position receptors of the articular segments.
- The VATER PACINI corpuscles, at the ligament level, are acceleration receptors.
- GOLGI’s tendon organs, located in muscle tendons and intramuscular aponeurotic partitions are specifically stimulated by muscle stretching.
- The neuromuscular spindles located in the fleshy part of the muscle give the indication of muscle length.
- There are also paciform corpuscles, free terminations, cutaneous receptors and intrinsic receptors of the vascular walls.
Effectors
The effectors concerning joint mobility are on the one hand the local periarticular and regional muscles responsible for posture, and on the other hand the circulatory system responsible for trophicity.
Nerve centers
Medullary and cortical ganglia.
A joint never acts in isolation, it participates in an articular complex whose unity is linked to physiology:
• At the level of the spine, a vertebra never dies in isolation from another; a whole functional whole synergistically modifies the ratio of these bone parts.
• At the level of members, obvious complexes are sometimes arbitrarily restricted; thus articular changes in the bones of the foot affect not only the tibiotarsal joint, but also the lower and upper fibulae.
All the modifications of an articular complex, as a rule asymmetric, constitute the distortion of this complex, either as a mechanism of adaptation to a physiological or traumatic stress, or as a dynamic correction mechanism. The permanence of the distortion, while the stress has ceased, is a sign of pathological joint blockage, hyper pressure in the cartilage.
This joint blockage is the cause of mechanical stress on the cartilage and thus constitutes the beginning of osteoarthritis degeneration.
However, this pathological condition can be recognized in its early stages because it is reversible and its resolution constitutes a preventive action against the mechanical causes of osteoarthritis.
This condition was highlighted by John Mac Mennel and published in 1964 in Long Beach, he calls it “Joint Dysfunction”. It means a loss in the play of the joint, which can be produced by the action of voluntary muscles.
Recognizing the dysfunction can only be done by clinical means, it does not cause any biological alteration that laboratory methods can detect.
The detection and treatment of joint dysfunction therefore depends on a method of clinical examination based on anatomical knowledge of the full range of normal motion for each individual synovial joint.
All normal movements in the mobility of the
“Joints are accomplished without pain; if there is pain, this is an indication that the movement is defective, the movements of the play of the joint are independent of the voluntary muscles. These movements are of very small amplitude, but very precise. It is on their integrity that the accomplishment of easy and painless movements to their full extent depends. Their integrity and not their amplitude is the basis of their importance.
It is the sum of joint play movements and voluntary stretch movements that cause the movements of living anatomy. Any restriction of mobility leads to tissue damage to the cartilage, generating the mechanical causes of the degenerative phenomena of osteoarthritis.
Doctor René HERNANDEZ
ARTHROSIS AND FREE RADICALS
Physiopathology of osteoarthritis by Doctor Jean-Claude PAWLAK
Osteoarthritis is defined as a degeneration of the articular cartilage characterized by cracks from the surface to the depth and progressive loss of cartilage. This non-vascularized hyaline connective tissue plays a fundamental role in the absorption of shocks linked to movement and the distribution of pressures. It is made up of an extracellular matrix and a single type of cell: chondrocytes.
The extracellular matrix consists of a dense structure of collagen fibers and proteoglycans, themselves made up of glycosaminoglycans, characterized by the presence of negative groups attracting positive Ca2 + and Na + ions. This cationic presence allows water to enter the cartilage, giving it a remarkable intratissular pressure regulation activity. The chondrocytes, devoid of vascularization, function in autarky and anaerobic conditions and feed on the synovial fluid. They have the ability to activate to synthesize their extracellular matrix, enzymes and cytokines. Cartilage regeneration is a regulatory phenomenon that opposes the destruction of chondrocytes.
In mature adult cartilage, everything is perfectly self-regulated: the survival of chondrocytes, the synthesis / destruction of the matrix. When this balance is upset and the destruction of cartilage cells outweighs its regeneration, the process of cartilage damage is set in motion.
The pathophysiology of osteoarthritis is based on two main theories. The theory of mechanical stress can explain the appearance of cracks by rupture of collagen fibers, causing hyperhydration, softening of the articular cartilage with formation of edema and biomechanical modifications. As the regulation of intratissular pressures is altered, the cartilage weakens and cracks. These disturbances lead to overproduction and overactivity of chondrocytes which activate the regeneration of the matrix in order to rebuild the cartilage. This hyperexcitability of the metabolic system develops a reactive osteophytosis, more commonly called “parrot beaks” and generates degradative enzymes of the matrix (collagenases, stomelysins), free radicals, nitrogen monoxide.
We then approach the second concept, the cell theory, extremely complex, which explains the degeneration of cartilage by cellular imbalances. The mechanical stimulus could in fact directly overactivate the chondrocytes. The acceleration of the chondrocyte metabolic system will produce excess pro-inflammatory mediators, generate degradation products of the extracellular matrix and release free radicals. The latter then participate in the inflammatory phenomenon, which in turn weakens the cartilage and also activates the chondrocytes.
The onset of osteoarthritis is not always known. It is certainly linked to the conjunction of these two theories but can also come from hereditary factors and of course from cell aging. The irreversibility of the disease stems from the complexity of the biochemical mechanisms, all intertwined with each other, all drawn into a vicious circle.
Epidemiological data
From an epidemiological point of view, many studies have provided important conclusions, opening new perspectives in the treatment and prevention of osteoarthritis. Patients with osteoarthritis have been shown to have:
- a low serum Selenium (Se) level,
- a higher serum malondialdehyde (MDA) level than others,
- activities of catalase and glutathione peroxidase also higher than the others.
These data indicate the presence of significant oxidative stress: a reduced selenium level is indeed a sign of a prooxidant / antioxidant imbalance, i.e. an excess of free radicals, selenium being a co-factor of the glutathione peroxidase, an enzyme that protects membranes against oxidation.
The MDA, which rate is higher in patients with osteoarthritis, is a degradation product of lipids, more particularly polyunsaturated lipids of cell membranes and lipoproteins. It is a marker used to measure the intensity of oxidative stress. As for catalase and glutathione peroxidase, an increase in their enzymatic activity also reveals the presence of oxidative stress.
Radical species, derived from oxygen (superoxide anion, hydroxyl radical, singlet oxygen) or nitrogen (nitrogen monoxide), are not only toxic to the organism: a small amount is produced by physiological mechanisms to fight against bacteria and participate in the regulation of cellular functions. When the quantities produced are excessive, oxidative stress appears. Inflammation is notably the site of an overproduction of radical species, directly produced by activated phagocytic cells. The NADPH oxidase complex is activated as well as superoxide dismutases and NO synthases. This results in an explosive production of superoxide anion, hydroxyl radical, singlet oxygen, nitrogen monoxide. During oxidative stress, a set of genes are brought into play to activate the synthesis of antioxidant enzymes. However, radical species can also activate genes for cellular functions other than those for antioxidant control. The genes for cytokines, collegenase, lipoprotein lipase and phospholipase can thus be activated by the active species of oxygen. These inflammatory vectors worsen the damage to the interarticular tissue. In vitro studies on interleukins-1, more particularly on IL-1 • (produced locally by chondrocytes during osteoarthritis), have shown their ability to inhibit the synthesis of collagen and proteoglycans, the main constituents of the extracellular matrix, but also their ability to inhibit the enzymes involved in the production of glycosaminoglycans. IL-1 is also thought to induce the production of pro-inflammatory prostaglandins. It has been shown that in high doses, IL-1 causes the death of chondrocytes, by complex mechanisms involving nitric oxide and free radicals.
Free radicals / Antioxidants
These epidemiological data and the biological understanding of the destructive mechanisms have made it possible to direct research towards the beneficial action of natural antioxidants and anti-inflammatories, and towards glucosamine, a substance used by chondrocytes to synthesize their extracellular matrix.
The first solution to control the rate of free radicals is the consumption of antioxidants.
- A study on the course of joint deterioration showed that patients with osteoarthritis consuming large amounts of antioxidants had a slower course than in patients who consumed little or no.
- Several studies have shown that supplementation with antioxidant vitamins C and E has a beneficial effect in the treatment or prevention of osteoarthritis.
- A study from the Framingham Osteoarthritis Cohort Study (consumer study on a total of 640 people with osteoarthritis of the knee) showed the preventive effects of a high vitamin C supplementation, and relatively less vitamin E and betacarotene.
- Studies specific to vitamin E have underlined its beneficial activity on the production of glycosaminoglycans, constituent cells of cartilage, and its inhibitory power in the process of cartilage destruction. In addition, a comparative study has shown an effectiveness of vitamin E very close to that of a Non-Steroidal Anti-Inflammatory Drug.
The second solution involves the action of metalloenzymes, enzymes whose action is catalyzed by a metal. Manganese superoxide dismutases (MnSOD), for example, allow the superoxide anion to be removed by a dismutation reaction. Selenium glutathione peroxidases (GPX), for their part, make it possible to eliminate radicals of the hydroxyl type but also organic peroxides. The action of these GPXs is very dependent on the selenium intake. Supplementation with trace elements would improve the activity of these metalloenzymes and thus fight against the effects of oxidative stress.
Research on other substances such as glucosamine, chondrotoin sulphate and S-adenosyl methionine have made it possible to consider other strategies. It has been shown that a supply of glucosamine allows the body to synthesize proteoglycans and glycosaminoglycans, to activate chondrocytes and to inhibit the action of destructive enzymes of the collagenase or phospholipase type. Chondrotoin sulfate, although its absorption is lower than that of glucosamine, has beneficial effects on stimulation of the production of matrix cells and hydration of the joint. A comparative study of the effects of S-adenosyl methionine compared to those of an anti-inflammatory (naproxen) showed a comparable action of the two products, the action being faster with the taking of anti-inflammatory, but the result at the end of treatment remaining the same.
To conclude, let us specify that the current treatment of osteoarthritis is mainly intended to relieve pain and slow down the deterioration of the cartilage. It seems essential for this to fight against the destructive effects of free radicals, by helping the body to build up its antioxidant barrier by providing antioxidant vitamins (A, C, E), carotenoids, flavonoids and essential fatty acids with anti- inflammatory (Omega-3).
The action of substances such as glucosamine, chondrotoin sulphate and S-adenosyl methionine offer new perspectives not only in the management of pain but also in the reconstruction of cartilage.
Doctor Jean-Claude PAWLAK
ARTHROSIS
Fouling pathology by Doctor Eric MENAT
Osteoarthritis is a degenerative disease linked to the wearing away of cartilage. This wear can be seen on standard x-rays. But the pain never has to do with the amount of wear and tear seen on the radio. Some people have severe bone damage and little pain, while others have very debilitating pain despite fairly moderate wear and tear on their joints.
Several types of osteoarthritis
If you have persistent pain, always located in the same joint, it is likely that you have classic degenerative osteoarthritis.
But if the pain affects several joints, the localization is variable depending on the day, you probably have a rheumatic ground linked to a “fouling” of the joints as defined by Dr Jean SEIGNALET.
The goal of the therapist is to limit the progression of osteoarthritis but also to treat the symptoms and in this case the pain.
However, in the event of pain affecting multiple and variable joints, if the fouling is indeed the cause, analgesics will be insufficient, while simple and natural methods can be particularly effective.
1) “Cleanse” the body with a diet
As with any fouling pathology, it is with food that we will have the best results. Start with a vegetable diet. For 1 to 3 days depending on your motivation, you will eat only cooked vegetables, in the form of soup, broths or vegetables with a little olive oil and salt, but avoiding any other seasoning.
You will thus make 4 to 6 meals of vegetables (quantities at your convenience).
You can drink water, herbal teas or green tea only between meals.
For the next 4 days, choose a totally vegetarian diet by combining vegetables with gluten-free cereals and pulses. That is to say: quinoa, rice, potatoes, lentils as well as rice cakes and flower bread (buckwheat cakes).
You can also eat cooked fruit.
2) Move towards a “hypotoxic” diet
Thirdly, you will diversify your diet by avoiding reintroducing:
baked wheat (bread, biscuits and pastries, pie or pizza dough …)
all derivatives of cow’s milk
too sweet desserts
foods cooked at high temperature (fried foods, grilled meats, etc.)
Here is an example of meal planning
Morning:
Option A:
Rice or buckwheat pancake with 2 boiled eggs
Option B:
1 plain soy yogurt + 1 compote + ground wheat germ
With a handful of almonds and some dried fruits (apricots, prunes …)
Midday:
Raw vegetables with a rapeseed oil vinaigrette
Steamed fish or Baked poultry + various steamed vegetables with a little olive oil and herbs 2 rice cakes – 1 compote
4 p.m: raw fruits and dried fruits
Dinner:
Soup or raw vegetables, Rice or quinoa + lentils (or other pulses) + vegetables 1 tablespoon rapeseed oil, 1 sheep or soy yogurt
Necessary food supplements
In case of fouling, the priority is to strengthen the intestinal barrier. We use fairly systematically:
• a probiotic to improve the intestinal flora,
• chlorophyll which absorbs toxins and helps to maintain a healthy intestinal lining.
If the fouling phenomena are marked, it may be necessary to “drain” the body.
• I always give priority to Aloe Vera which is a wonderful depurative,
• If the presence of xenobiotics (chemical molecules or heavy metals linked to environmental or food pollution) is suspected, pure chlorophyll will be replaced by a more complete chelator.
In all the case, since we are talking about joint damage, it is necessary to act directly on the symptoms by:
• herbal medicine very effective on pain
• oligotherapy (see box)
• joint nutrition and in particular glucosamine and silica which have shown their role in the prevention of osteoarthritis.
Box on oligotherapy
Catalytic oligotherapy is a method used for decades by homeopaths to act on various pathologies.
This method had its heyday in the field of osteoarthritis thanks to Dr. Picard who proposed an alternative treatment of different trace elements.
We mainly use oligosols which come in ampoule form.
Here is a “recipe” which has proven itself:
Take a dose or an ampoule of the following OLIGOSOLS in the morning on an empty stomach and at bedtime:
Monday and Thursday:
Morning: Copper-Gold-Silver Evening: Potassium
Tuesday and Friday:
Morning: Manganese-cobalt Evening: Fluorine
Wednesday and Saturday:
Morning: Sulfur Evening: Magnesium
Here, it is not the nutritional role of trace elements that we are looking for, but their “catalytic” role, that is to say of stimulation, of facilitation of bone metabolism.
Doctor Eric MENAT
ARTHROSIS AND CHRONOBIOLOGY
by Professor Jean-Robert RAPIN (Dpt. of Pharmacology, University of Burgundy)
Osteoarthritis: a degenerative disease
Osteoarthritis is a degeneration of the cartilage without infection or inflammation. Cartilage is the site of intense activity with the multiplication of cells; chondrocytes which opposes their destruction and synthesis by these cells of many metabolites such as the ground substance consisting of a polymerization of glucuronic acid and N acetyl glucosamine. During degeneration, proteolytic activity takes precedence over anti-proteolytic activity, resulting in depletion of chondrocytes and a decrease in their number. The thickness of the cartilage decreases and the dead cells as well as fragments of cartilage that are free will lead to inflammatory outbreaks resulting in a local rise in temperature, hypersecretion of fluid and swelling of the joint. In addition to these phenomena, bone proliferation under the cartilage causing deformities.
Pain apart from inflammatory attacks is mechanical and has the following characteristics:
- it is triggered and made worse by movement
- it ceases or subsides during rest
- it hinders falling asleep and causes nocturnal awakenings
- it is weak in the morning, and it increases during the day with the maximum in the evening
There is no biological marker and the diagnosis is essentially clinical with radiological confirmation.
The origin is discussed, but there is always a genetic factor, on which risk factors such as overweight, repetitive trauma (sport, work, etc.), menopause (women are more affected than men), ageing etc. are added.
Since this is a degenerative disease, arthritis lesions are irreversible and, in addition to the deformities, lead to joint stiffening progressing to impotence. The goal of all therapy is to slow down the rate of growth and decrease painful sensations.
Osteoarthritis in relation to our biological rhythms
All cellular activities are subject to important biological rhythms whether they are circadian over 24 hours, monthly or annually. Virtually all diseases, including osteoarthritis, are linked to biological rhythms with the definition of a new discipline of chronopathology. This corresponds to the study of periodic variations in the signs and symptoms of a disease in a patient or in a group of patients. In addition, chronopathology corresponds to the disturbances of our biological clocks. Currently in the case of osteoarthritis, it is not possible to say that the origin of the disease is linked to changes in the clocks, but it is certain that there is a disorder that must be known in order to predict adapted therapies (chronotherapy).
Without going into detail, biological clocks allow us to adapt. Thus during the day, all cellular functions are focused on defense against aggression, while during our sleep, functions are focused on cell renewal (multiplication, renewal of membranes, etc.).
For higher organisms like humans, cellular biorhythms are under the control of a main clock represented by specialized hypothalamic structures: the supra chiasmatic nuclei in relation to retinal nerve cells sensitive to the day / night rhythm and to the base of activity of the hypothalamic-adrenal axis. This primary clock controls and receives information from secondary clocks which include the limbic system (behavior and mood), neuroendocrine systems, and the pineal gland (melatonin secretion).
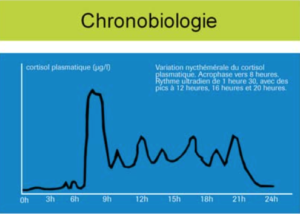
The hypothalamic-adrenal axis ensures the secretion of cortisol. This secretion is maximum in the morning (at 8 o’clock) then peaks are observed every 90-120 minutes with 4 main peaks at 8 a.m., 12 p.m., 4 p.m. and 8 p.m. There is no production of cortisol at night.
This cortisol, our natural corticosteroid provides (especially in the morning when secretion is maximum):
• inhibition of prostaglandins and leukotrienes (pain relief),
• immunosuppression (decrease in lymphocyte production),
• stopping cell multiplication,
• expression or inhibition of protein synthesis with a corollary of activation or inhibition of enzymes,
• modulation of the activity of our main hormones such as insulin,
• modulation of metabolisms such as calcium phosphorus.
In arthritis patients, apart from inflammatory attacks, the morning secretion of cortisol is reduced, which results in:
• the onset of pain that intensifies during the day since cortisol will be weaker and weaker (1),
• immunosuppression with an imbalance between interleukins. IL6 which is a regulator of the hypothalamic-adrenal axis is increased (2). We can nevertheless observe a profound modification in the time of IL secretion (3),
• a change in parathyroid hormone secretion and its circadian rhythm with the consequence of impaired bone function (4),
• an increase in the secretion of prolactin, which is a pro-inflammatory hormone (5).
All of the work shows that there are profound changes in circadian rhythms in arthritis patients (6).
Melatonin
Normally it is secreted at night with a peak around 2 a.m. In arthritis patients, all studies show an increase in melatonin production both during the peak and later at night (7, 8, 9). This change in the circadian rhythm of melatonin is related to changes in bone metabolism.
Local rhythms in the cartilage
Undoubtedly under the dependence of cortisol, there are local modifications concerning ions, trace elements and pH. The latter, measured in synovial fluid, is very acidic in the morning and rises during the day. As the activity of proteases is maximal in an acidic environment, degeneration is observed especially in the morning. In addition, proteases are Zinc enzymes and are partially inhibited by copper. Finally, the multiplication of chondrocytes and the synthesis of the protein framework and the ground substance take place at night.
In practice, what nutritional advice to give?
1) Give probiotics in the morning in order to rebalance the intestinal immune function, which results in a decrease in pro-inflammatory interleukins IL6 in particular,
2) Give omega 3 fatty acids (EPA) in the evening to reduce the synthesis of group 2 prostaglandins (PGE2) responsible for the painful sensation,
3) Alkalize the body with fruits and vegetables. Bicarbonated water, taken in the morning, gives an identical effect but with a high salt intake,
4) Take calcium and magnesium in the morning in the 3/1 ratio,
5) Take glucosamine,
6) Take anti-free radicals, to prevent the onset of inflammatory flare-ups and to limit their effects. Vitamins E and C, polyphenols, flavonoids, selenium and manganese.
The use of these nutraceuticals decreases the progression of degeneration and provides comfort by reducing painful sensations.
Professor Jean-Robert RAPIN
References:
1. Cutolo M., Villagio B., Otsa K., et al
Altered circadian rhythms in rheumatoid arthritis patients play a role in the disease’s symptoms Autoimmun Rev. 8 (2005) 497-502
2. Mastorakos G., Ilias I.
Relationship between interleukin 6 and hypothalamic-pituitary-adrenal axis hormones in rheumatoid arthritis. Rheumatol 59 (2005) suppl2 75-79
3. Li S., Lu A., Li B. Wang Y.
Circadian rhythms on hypothalamic-pituitary-adrenal axis hormones and cytokines of collagen induced arthritis in rats. J. Autoimmun. 4 (2004) 277-285
4. Fraser W.D., Ahmad A.M., Vora J.P.
The physiology of parathyroid hormone and its potential as a treatment for osteoporosis Curr. Opin. Nephrol. Hypertens. 13 (2004) 437-444
5. Zoli A., Lizzio M.M., Ferlisi E.M., et al
ACTH, cortisol and prolactin in active rheumatoid arthritis Clin. Rheumatol. 4 (2002) 289-293
6. Cardinali D.P., Esquifino A.I.
Circadian disorganization in experimental arthritis Neurosignals 6 (2003) 267-282
7. Cutolo M., Maestroni G.J., Otsa K. et al
Circadian melatonin and cortisol levels in rheumatoid arthritis patients in winter time: a north and south Europe comparison Ann Rheum. Say. 64 (2005) 212-216
8. Cardinali D.P., Garcia A.P., Cano P. et al
Melatonin role in experimental arthritis
Curr. Drugs Target Immune Endocr. Metabol. Disord. 4 (2004) 1-10
9. Ostrowska Z., Kos-Kudla M., Swietochowska E., et al.
The relationship between bone metabolism and other hormones in sham-operated and pinealectomized rats Endocrin. Regul. 37 (2003) 211-224
ARTHROSIS and ESSENTIAL OILS
by Doctor Jean-Pierre WILLEM
Rheumatism refers to acute or chronic conditions, characterized by pain and fluxion located on the osteoarticular system. In practice, this definition only concerns acute injuries. In fact, degenerative pathologies, such as osteoarthritis or osteoporosis, are only painful by the side reactions they cause, in particular at the muscular level.
Osteoarthritis is therefore a chronic degenerative and non-inflammatory condition of the joints. This disease involves erosion or destruction of cartilage, but also damage to the bone and synovium. It is the most common of all joint diseases. We distinguish, classically, primary (idiopathic) osteoarthritis and secondary osteoarthritis that many biological and traumatic phenomena can trigger. Pain worsened by exercise is the earliest symptom. Radiologically, there is a pinching of the joint space (which corresponds to areas of destroyed cartilage), condensation of the subchondral bone, bone geodes, osteophytes.
The symptomatology of osteoarthritis is almost the opposite of that of inflammatory rheumatism:
• pallor,
• coldness of the areas concerned,
• loss of bone and / or cartilage material,
• almost no pain,
• frequent improvement by pressure and local heat,
• sometimes sensitive to barometric variations.
Impotence is slower to set in, and sometimes requires surgery.
In practice, the two symptoms are intertwined (example: arthritis outbreak on the background of osteoarthritis). We will say for simplicity that:
• osteoporosis is a bone disease,
• osteoarthritis is a condition of the cartilage,
• arthritis is a condition of the synovium,
• Inflammation of the tendons (tendonitis) is frequently associated with these joint disorders.
In addition to the anxiety generated by pain, deformity and functional impotence reveal the specter of aging.
Phyto aromatherapy offers an impressive number of plants known to be active to very active on almost all the symptoms encountered (pain, inflammation, edema, deformation, anxiety …).
The interest of such treatments lies above all in:
• its good efficiency,
• its relative harmlessness compared to non-steroidal anti-inflammatory drugs and corticosteroids,
• its beneficial influence on extra-rheumatic manifestations (eg meadowsweet is anti-inflammatory and diuretic).
TREATMENTS…
Physical treatments
Let us cite jumble of physiotherapy, osteopathy, massages, applications of liniments based on mud, clay, algae, essential oils.
Rest, even immobilization (sometimes surgical: arthrodesis).
Thermal cures.
The correction of dietetics
From osteoarthritis to cancer via gout or osteoporosis, all pathologies benefit more or less from an adaptation of the nutritional regime and the intake of vitamins, trace elements, poly fatty acids. -unsaturated.
Energy treatments
Acupuncture, homeopathy, magnetotherapy are precious allies.
Psychotherapeutic treatments
The questioning of rheumatic patients often reveals a psychorigid profile, of which joint stiffness is only a physical expression.
This rigidity makes them little adaptable, they doubt themselves, devalue themselves and become depressed.
Anxiolytics and antidepressants are also widely prescribed by rheumatologists.
Revaluing psychological help and offering the patient the possibility of freeing himself from dogmatic beliefs will prove to be relevant.
Phyto-aromatherapy treatments
We report here a list of medicinal plants and Essential Oils commonly used in rheumatic diseases, whose reliability is certain but whose prescription requires a certain rigor, almost homeopathic, in the questioning of the patient. The notion of the patient’s “receptivity” to a treatment takes on its full meaning here. In addition, many plants are dynamically active on several symptoms at the same time, which makes their classification difficult.
The action of Essential Oils is remarkable, but the use requires a solid knowledge of the contraindications and undesirable effects.
E.O analgesics
• E.O. of Ajowan
• E.O. of exotic Basil
• E.O. of yellow birch
• E.O. of Wintergreen
• E.O. of Aspic Lavender (Lavandula latifolia)
• E.O. of sweet Bay
• E.O. of Peppermint
E.O. camphor analgesics
• E.O. of Achille millefeuille
• E.O. of Camphor tree from Japan
• E.O. of Rosemary with camphor
E.O. analgesics with calming aim
• E.O. Camomile
• E.O. of Cumin of the meadows
• E.O. of True Lavender, Lavandin (Lavandula burnatii super)
• E.O. of Lemon Litsea
• E.O. Small grain bitter orange
E.O. anti-inflammatory drugs
• E.O. of exotic Basil
• E.O. of Camomile
• E.O. Java Lemongrass
• E.O. of black spruce
• E.O. of Tarragon
• E.O. of Lemon Eucalyptus
• E.O. of Sweet fennel
• E.O. of Lavandin (Lavandula burnatii super)
• E.O. of lemon mint
Several formulations in aromatherapy
1) Cutaneous use – 1st formula
E.O. Eucalyptus CT cryptone 0.5 ml
E.O. Gaultheria procumbens 2 ml
E.O. Lavandula super acetate 4 ml
E.O. Satureja montana 1 ml
E.O. Thymus CT thujanol 0.5 ml
E.O. Thymus saturated 2 ml
Neutral gel or vegetable oil in sufficient quantity for 100 ml
3 to 4 local applications per day for 15 days (continue if necessary), and, in addition,
2nd formula
E.O. Picea mariana 3 ml
E.O. Pinus sylvestris 7 ml
V.O.* Hazelnut in sufficient quantity for 30 ml
6 to 8 drops in adrenal unctions twice a day
*V.O. : Vegetable Oil
3rd formula
with analgesic and antirheumatic aims:
E.O. Eucalyptus polybracts (cryptone) 4 ml
E.O. Thymus vulgaris thujanol 2 ml
E.O. Satureja montana (carvacrol) 2 ml
V.O. Corylus avel. in sufficient quantity for 30 ml
2/4 applications per day, for 2 weeks to renew if necessary
2) Oral route – 1st formula
E.O. Eucalyptus dives 20 mg
E.O. Juniperus communis sub-species communis 20 mg
E.O. Mentha piperita 20 mg
E.O. Ocimum basilicum sub-species basilicum 20 mg
E.O. Petroselinum crispum 20 mg
Excipient 320 mg
to make a capsule n°0 Dt 40 – 1 capsule morning and evening before the meal for 20 days (continue if necessary).
2nd formula – hepato-pancreatic stimulant aim:
E.O. Juniperus com. ssp alpina 25 mg
E.O. Mentha x piperita 25 mg
Excipient in sufficient quantity for 1 capsule n°2, n°CX - 1 capsule 3 times a day for 20 days
Homeopathy
Homeopathy can only act on the painful element.
This is not a list of drugs indicated according to pain but rather osteoarthritis as a degenerative disease. The presence of various calcium salts is explained by the pathophysiology, which is in the foreground here since the treatment aims to improve the condition of the bones, more than to respond to symptoms.
Joint pains, deformities, functional impotence are the signs of the degenerative rheumatism or osteoarthritis; the pains are worsened with support, with the effort, and are improved at rest, at night, even if the morning “rusting” is difficult.
The slow and gradual onset of pain and impotence as well as their worsening in humidity testify to a ground which will be treated by drugs of the sycotic reaction mode (Thuja and Natrum sulfuricum in weekly dose).
• if the pain is improved by rest and immobility, compression, and aggravated by movement, shaking: Bryonia 9 CH, 5 sugard pills 1 or 2 times a day.
• if the pain is aggravated by rest and humidity and improved by slow movement and heat: Rhus toxicodendron 9 CH and Radium bromatum 9 CH, 5 sugard pills 1 or 2 times a day.
Other remedies
Calcarea carbonica: osteoarthritis in a patient with large bones and rigid joints; nodules; worsening by humidity; improvement when stretching.
Calcarea fluorica: osteoarthritis in a patient with ligament hyperlaxity; importance of osteophytes and exostoses.
Calcarea phosphorica: osteoarthritis in an elongated patient with flexible joints; preferential locations at the level of the sutures and symphyses, in particular at the level of the sacroiliac joint and the pubic symphysis; feeling of numbness in the extremities; stiffness; worsening by snowy or stormy weather.
Causticum: osteoarthritis complicated by tendon contractures.
Phosphorus: osteoarthritis with a tendency to osteonecrosis.
Argentum metallicum: arthralgias with a feeling of tightness due to cartilage damage.
Hekla lava: medication to be prescribed on the concept of osteophytes, exostoses.
Kalium carbonicum: low back pain; hip pain radiated to the knees; feeling of general weakness.
Natrum sulfuricum: infiltration of the joints; obesity; worsening by wet weather.
Ruta graveolens: lesions of the periosteum.
Silicea: osteoporosis.
Sulfur: rhizarthrosis; tendency to joint effusions; burning pain aggravated by heat; worsening from standing; alternating rheumatic pain with diarrhea or eczema; sulfur has an essential role in the metabolism of bone.
Sulfur iodatum: most of the time, when Sulfur is indicated, it is preferred to replace it with Sulfur iodatum, which does not give rise to side effects.
Thuya occidentalis: osteoarthritis with a sensation of glass bones, bones that are going to break; worsening by humidity; improvement in stretching; possibly, gynoid obesity.
Standard prescription:
Calcarea phosphorica 7 CH,
Causticum 5 CH,
three granules of each alternating three times a day until improvement.
Doctor Jean-Pierre WILLEM
CONCLUSION
Osteoarthritis from different points of view
The various articles on osteoarthritis show us that, before the final term of surgical and prosthetic correction, there are a multitude of therapeutic routes likely to improve functional joint comfort.
This multitude of treatment proves, if it were necessary, that the origin of osteoarthritis is multifactorial and that many elements are often wrongly overlooked (who thinks of the intestinal flora in a patient with osteoarthritis?)
Whether the etiology is mechanical, whether the acid-base imbalance or oxidative stress are preponderant, whether the theory of fouling and the proliferation of free radicals are or are not associated with genetic disorders, the prevention of functional disorders and pain are part of the fight for the well-being of the individual; because it must be recognized that treatments for osteoarthritis are not legion when the pathology is installed. It is by being present as early as possible that we will be able to limit the development of clinical signs and joint degradation.
Doctor Roger LECURIEUX-CLERVILLE